Scriptsure integrates with Cover My Meds to provide information about Prior Authorizations.
Scriptsure has provided the following documentation for Cover My Meds.
A complete user guide is also available from CoverMyMeds: CoverMyMeds App User Guide.pdf
How do Prior Authorizations work?
Scriptsure has the ability to link to CoverMyMeds for prior authorizations.
When appropriate, an agency may get a prompt to enable prior authorizations. The prompt looks like this: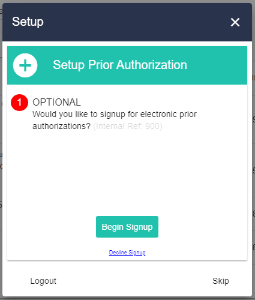
If the integration is desired, click Begin Signup and you will be walked through prompts for setting it up.
If the integration is not desired, click Decline Signup.
If you are not sure, click the Close X or Skip. You will receive the prompt again the next time you login to Scriptsure.
You can also Sign Up for Prior Authorizations by going to the Settings menu: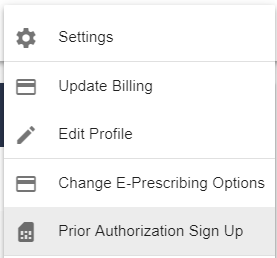
Prompts you may see in the Sign Up (RH NOTE: Update this when we have documentation from Scriptsure!)
|
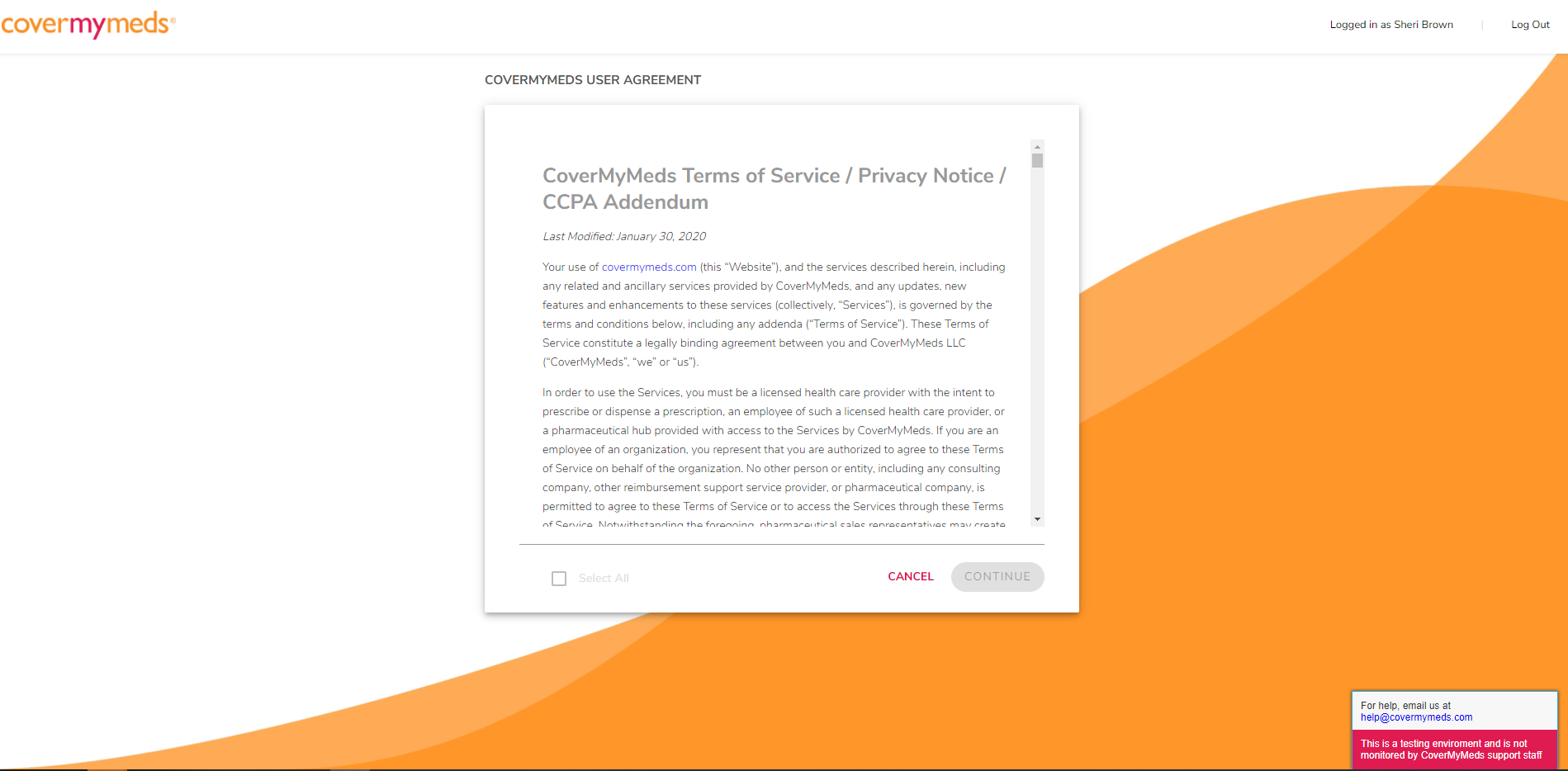
Read Terms |
|
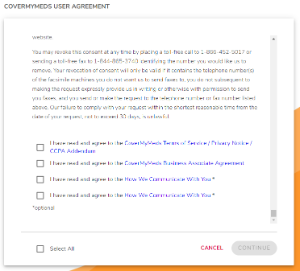
Scroll to bottom, check boxes and click Continue |
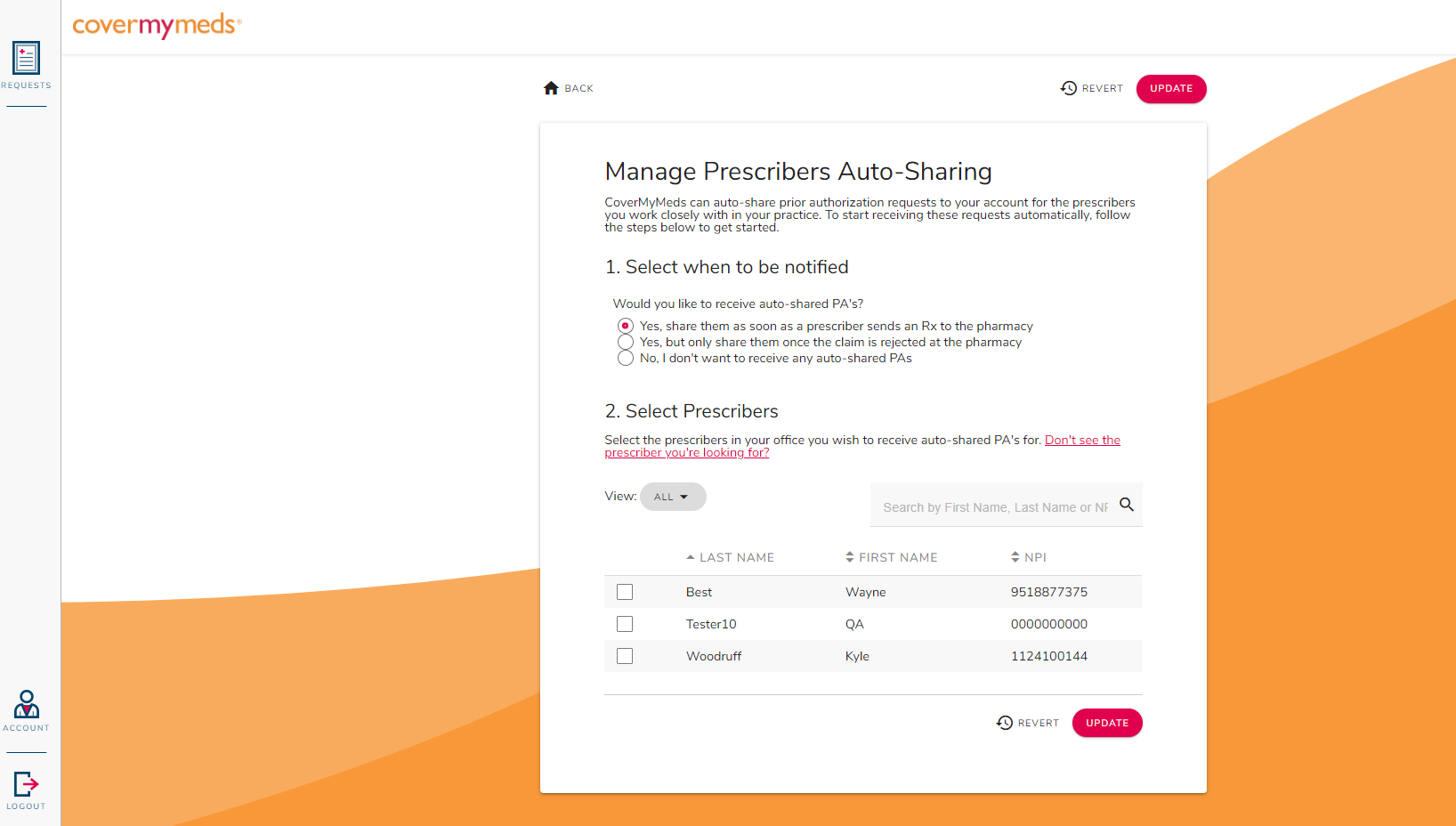 |
Select when to be notified and which Prescribers you which to receive notifications about. Click Update |
|
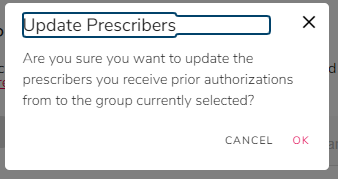
Click OK to confirm the update |
|
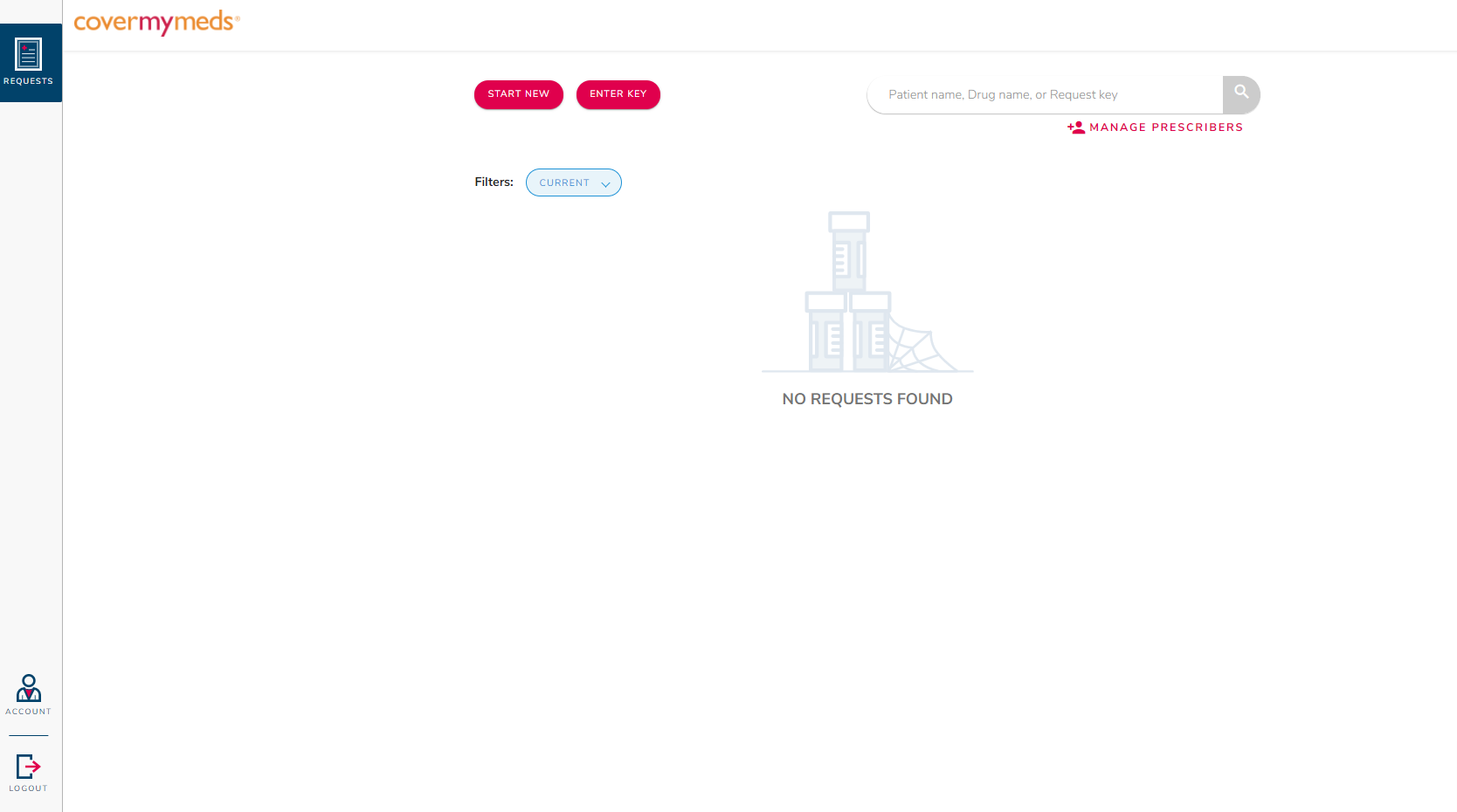
You are then shown the CoverMyMeds dashboard. |
From this point, it is the same interface you are used to in CoverMyMeds.
See Cover My Meds documentation (above) for additional information on using Cover My Meds.
Our CoverMyMeds Prior Authorization account is under the administrator. Will it work for my Prescribers?
The CoverMyMeds interface in Scriptsure is the same interface CoverMyMeds provides outside of Scriptsure.
The administrator may go into CoverMyMeds as a supporting user and select the prescribers that they want to manage. They will need to have Prescribe Using access within Scriptsure to facilitate that.
See Cover My Meds documentation (above) for additional information on using Cover My Meds.