Patient Signatures
Users have the ability to apply additional signatures to their progress notes. These signatures can be for patients, guardians, or additional signers. Once signatures are configured, they show at the bottom of the progress note.
 CT|One Configuration
CT|One Configuration
CT|One patient and additional signatures are configured under Note Types. There is a new column in the Note Type editor for Signatures.
Signatures can be configured for all the service types for the note type, or specific configurations per service type.
For more information check out the Note Type configuration here.
 myAvatar and myEvolv Configuration
myAvatar and myEvolv Configuration
myAvatar and myEvolv signatures are applied and configured within Custom Note Sections. These are imported and use the configuration from the EHR.
For more information check out the Custom Note Section article here.
Patient View
The patient view is configured on Note Type sections and Custom Note Section questions.
When a section is set to Include in patient view, that section will show in the Patient View for notes that are configured with Signatures.
Patient view is additionally set for Custom Note Sections per question type. You will not see the Include in patient view setting when you select a custom note section for your note since these are done per question type in the custom note section configuration.
For more information check out the Note Type configuration article Patient View section here.
Progress Note Editor
In the progress note editor, signatures display at the bottom of progress notes. Clicking sign takes you through the signature workflow, including the Who is signing configuration and the patient view displays.
Signature Workflow
Clicking Sign on a patient/additional signature box will follow this workflow:
- Patient-viewable sections are validated for required content.
- Additional information for who is signing can be added as needed.
-
Patient view displays, where all patient-viewable content except the signature is read-only.
Bells administrators configure which note sections are patient viewable. - Signatures are applied.
- All content in patient-viewable note sections is locked down and can no longer be modified.
- When done signing, the practitioner enters a PIN to resume control of the entire progress note.
- The therapist finishes the progress note, modifying any non-patient-viewable sections as necessary.
- The therapist signs the note.
A patient/additional signature can be removed once signed if a note needs to be further edited.
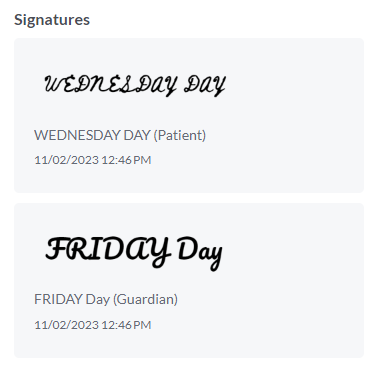
Once applied, the drawn or typed signatures show in the note.
For more information check out the Individual Progress Note Editor article here.
The patient/additional signature capturing has also been applied to the Bulk Sign, Group Note and Goal Tracking flows.